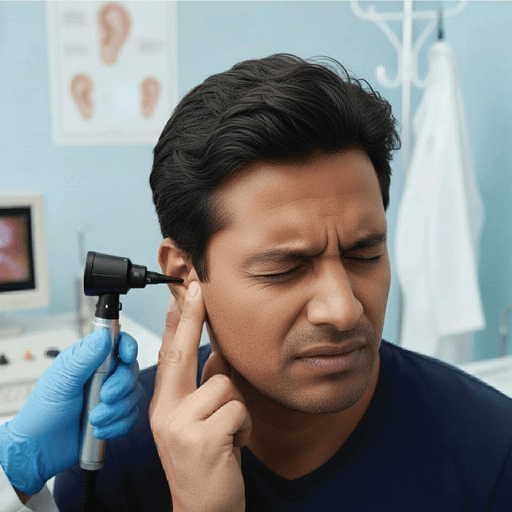
This minimally invasive procedure is designed to repair perforated eardrums and restore hearing function. Performed using a high-definition endoscope, the technique allows for enhanced visualization of the middle ear structures, ensuring greater precision and accuracy during surgery. The endoscopic approach enables access through the ear canal, eliminating the need for external incisions and resulting in no visible scars.
Compared to conventional methods, this advanced technique offers several benefits, including reduced surgical trauma, minimal postoperative discomfort, faster recovery time, and improved surgical outcomes. It is a safe and effective option for both adults and children, particularly those seeking quicker healing and better cosmetic results.
The focus of this approach is to deliver safe, effective, and patient-centered ear care by combining the latest surgical technology with a personalized treatment plan tailored to each patient’s condition and lifestyle, ensuring optimal hearing restoration and long-term ear health.

Functional Endoscopic Sinus Surgery (FESS) is a minimally invasive surgical procedure used to treat chronic sinusitis, nasal polyps, and blocked or poorly draining sinuses. The procedure is performed using a thin, high-definition endoscope that allows the surgeon to precisely visualize and remove obstructions within the nasal and sinus passages, all without any external cuts or scars.
By restoring normal sinus drainage and ventilation, FESS helps relieve nasal blockage, facial pressure, headaches, post-nasal drip, and recurrent sinus infections. Compared to traditional sinus surgery, FESS offers several advantages, including less pain, minimal bleeding, faster recovery, and improved breathing.
FESS is a safe and effective treatment option for patients who continue to experience symptoms despite medical management such as medications, nasal sprays, or antibiotics. The procedure significantly improves sinus health, overall comfort, and quality of life, allowing most patients to return to normal activities within a short period.

Sleep apnea screening is a crucial first step in identifying individuals who may be at risk for this potentially serious sleep disorder. The screening process typically involves a detailed assessment of common symptoms such as loud or chronic snoring, excessive daytime sleepiness, unexplained fatigue, observed pauses in breathing during sleep, gasping or choking at night, and morning headaches. In some individuals, poor concentration, irritability, and disturbed sleep patterns may also be early warning signs.
Healthcare providers often use validated screening tools such as the STOP-Bang Questionnaire and the Epworth Sleepiness Scale to evaluate the likelihood and severity of sleep apnea. These tools help determine whether further diagnostic testing, such as an overnight sleep study (polysomnography) or a home sleep test, is required.
Early screening plays a vital role in preventing the long-term health consequences of untreated sleep apnea, which can include high blood pressure, heart disease, stroke, diabetes, weight gain, and impaired cognitive and work performance. Timely identification allows for early intervention through lifestyle changes, medical therapy, or device-based treatments like CPAP, significantly improving sleep quality, overall health, and quality of life.

Ossiculoplasty is a surgical procedure performed to repair or replace the tiny hearing bones (ossicles) in the middle ear that are responsible for transmitting sound from the eardrum to the inner ear. Damage to these bones can occur due to chronic ear infections, trauma, or conditions such as cholesteatoma, leading to conductive hearing loss.
The goal of ossiculoplasty is to restore the normal sound conduction mechanism, resulting in improved hearing levels, clearer sound perception, and better speech understanding. By reconstructing or replacing the damaged ossicles with biocompatible prostheses or reshaping existing bones, the procedure provides a long-term solution for hearing loss caused by middle ear damage.
Ossiculoplasty is a safe and effective surgical option that can be performed alone or in combination with other ear surgeries, such as tympanoplasty or mastoidectomy. Successful outcomes significantly enhance communication ability, confidence, and overall quality of life for patients experiencing hearing impairment.

Mastoidectomy is a surgical procedure performed to remove infected or damaged air cells from the mastoid bone, which is located behind the ear. It is most commonly required in cases of chronic ear infections or the presence of cholesteatoma, a destructive growth that can damage ear structures if left untreated.
The primary goals of mastoidectomy are to eradicate infection, prevent serious complications, and protect vital structures of the ear and surrounding areas. By removing the diseased tissue, the procedure helps stop persistent ear discharge, relieve pain and discomfort, and reduce the risk of complications such as hearing loss, balance problems, facial nerve damage, or spread of infection to the brain.
Mastoidectomy also aims to preserve and, in many cases, improve hearing, while creating a safe and dry ear for long-term ear health. It is a safe and effective surgical option when conservative treatments fail, significantly improving comfort, function, and overall quality of life.

Septoplasty is a surgical procedure performed to correct a deviated nasal septum, the cartilage and bone that separates the two nasal passages. When the septum is significantly misaligned, it can obstruct airflow and lead to chronic nasal congestion, difficulty in breathing through the nose, snoring, recurrent sinus infections, facial pressure, and disturbed sleep.
The procedure involves straightening and repositioning the septum to restore proper airflow through the nasal passages. By correcting the structural blockage, septoplasty helps patients breathe more easily, sleep better, and experience long-term relief from nasal obstruction.
Septoplasty offers several long-term benefits, including improved nasal function, reduced sinus-related problems, better sleep quality, and enhanced overall comfort and quality of life. It is a safe and commonly performed procedure, often done as a day-care surgery with a smooth recovery when performed by an experienced ENT specialist.

Lobuloplasty is a simple and effective surgical procedure performed to repair torn, stretched, or split earlobes, most commonly caused by heavy earrings, accidental trauma, or long-term use of ear piercings. The procedure focuses on restoring the natural contour and symmetry of the earlobe, improving both function and appearance.
It is a quick outpatient procedure, usually performed under local anesthesia, with minimal discomfort and downtime. Patients can typically resume normal daily activities shortly after the procedure. Lobuloplasty not only enhances cosmetic appearance but also strengthens the earlobe, allowing for safe re-piercing once healing is complete, if desired.
This procedure is a safe and reliable option for individuals seeking a long-lasting solution to earlobe deformities, delivering natural-looking results and improved confidence.
Styloidectomy is a surgical procedure performed to remove or shorten an elongated styloid process, a thin bony structure located near the base of the skull. It is most commonly done to treat Eagle’s Syndrome, a condition in which an abnormally long styloid process or calcified ligament causes irritation of nearby nerves and blood vessels.
Eagle’s Syndrome can lead to symptoms such as persistent throat pain, facial or neck discomfort, difficulty or pain while swallowing, earache, headache, and a constant sensation of a foreign body in the throat. These symptoms can significantly affect daily activities, including speaking, eating, and overall comfort.
By surgically correcting the elongated styloid process, styloidectomy provides long-lasting relief from pain and discomfort, restores normal throat function, and significantly improves quality of life. The procedure is safe and effective when performed by an experienced ENT specialist, helping patients return to normal daily activities with improved comfort and confidence.

Tonsillectomy is a surgical procedure performed to remove the tonsils, which are lymphoid tissues located at the back of the throat. It is commonly recommended for patients suffering from recurrent tonsillitis, chronic or severe sore throats, frequent throat infections, or breathing difficulties, including sleep-disordered breathing or obstructive sleep apnea caused by enlarged tonsils.
By removing chronically infected or enlarged tonsils, tonsillectomy helps significantly reduce the frequency and severity of throat infections, decreases dependence on repeated courses of antibiotics, and improves overall throat health. In patients with airway obstruction, the procedure also improves breathing, reduces snoring, and enhances sleep quality.
Tonsillectomy is a safe and well-established procedure that can be performed in both children and adults. The long-term benefits include better overall health, improved daily functioning, fewer missed school or workdays, and a noticeable improvement in quality of life.
Myringotomy is a surgical procedure in which a small incision is made in the eardrum (tympanic membrane) to drain trapped fluid and relieve pressure caused by recurrent ear infections or persistent fluid buildup in the middle ear. In many cases, a tiny ventilation tube known as a grommet is inserted into the eardrum to allow continuous drainage, improve air circulation, and prevent fluid from reaccumulating.
This procedure is especially beneficial for children who experience frequent ear infections or hearing difficulties due to middle ear fluid, though it may also be recommended for adults in certain cases. By restoring proper middle ear ventilation, myringotomy helps improve hearing, reduce the frequency and severity of infections, and relieve ear discomfort.
Myringotomy is a safe and commonly performed procedure, usually done as a day-care surgery with minimal discomfort and quick recovery. It plays an important role in promoting long-term ear health, normal speech development in children, and improved overall quality of life.
Microlaryngeal surgery is a highly specialized procedure used to treat voice disorders caused by abnormalities such as vocal cord nodules, polyps, cysts, or early-stage tumors. The surgery is performed using a high-powered operating microscope and fine precision instruments, allowing the surgeon to work with exceptional accuracy while preserving the delicate structure and function of the vocal cords.
This minimally invasive technique helps restore normal vocal cord vibration, leading to clearer voice quality, improved vocal strength, and reduced hoarseness. It is particularly beneficial for professional voice users, such as teachers, singers, speakers, and individuals who rely heavily on their voice, as well as patients with long-standing or recurrent voice problems.
Microlaryngeal surgery is usually performed as a day-care (outpatient) procedure with minimal discomfort and downtime. Most patients experience significant voice improvement with proper postoperative voice care and therapy, resulting in better communication, confidence, and overall quality of life.

Skin allergy testing is a safe and reliable diagnostic method used to identify substances that may be triggering allergic reactions, such as dust mites, pollen, mold, pet dander, foods, or environmental allergens. The test involves applying small amounts of specific allergens to the skin—usually on the forearm or back—and observing the skin’s response for signs such as redness, swelling, or itching.
This testing method helps provide an accurate diagnosis, allowing doctors to identify the exact cause of allergy symptoms. Based on the results, a personalized treatment plan can be developed, which may include avoidance strategies, medications, or immunotherapy.
Skin allergy testing is a quick, outpatient procedure with minimal discomfort and excellent safety. It plays a key role in achieving better long-term control of allergy symptoms, reducing flare-ups, and improving overall comfort and quality of life for patients suffering from allergies.
Adenoidectomy is a surgical procedure performed to remove enlarged or chronically infected adenoids, which are lymphoid tissues located behind the nasal cavity. Adenoids play a role in immune defense during early childhood, but when they become persistently enlarged or infected, they can lead to significant health issues.
Enlarged adenoids can cause difficulty in breathing through the nose, persistent nasal blockage, loud snoring, disturbed sleep, mouth breathing, recurrent ear infections, hearing problems, and frequent sinus or throat infections, particularly in children. In some cases, chronic adenoid enlargement may contribute to sleep-disordered breathing or obstructive sleep apnea.
Removing the adenoids helps restore normal nasal breathing, reduce the frequency of ear and upper respiratory infections, improve sleep quality, and enhance overall growth, development, and quality of life in affected children. Adenoidectomy is a safe, commonly performed procedure, often done as a day-care surgery with minimal discomfort and quick recovery, allowing most patients to return to normal activities within a short time.